Quality of Life in Patients with Dental Prosthesis in South Indian Population – Chennai, Tamil Nadu: An Epidemiological Survey
Sharmila Hussain, Gayathri Sathyamoorthy
Department of Prosthodontics, Madha Dental College and Hospital – Kunrathur, Tamil Nadu, India
Submission: 01 June 2020; Revision: 22 June 2020; Acceptance: 29 June 2020
ABSTRACT
A questionnaire consisting of approximately 9 questions is prepared individually for patients and circulated in specified locality and the responses given by the patients are statistically analysed to determine the awareness about “QUALITY OF LIFE IN PATIENTS WITH DENTAL PROSTHESIS”. The patients are completely/partially edentulous and who are prosthesis wearers. About 179 patients were surveyed and analysed. Patients’ perceived Health-Related Quality of Life (OHRQoL) may be defined as a multidimensional construct incorporating at least three broad domains: physical, psychological and social functioning. In the dental field, assessment of an individual’s Oral Health-Related Quality of Life (OHRQoL) has been exponentially increasing during the last decade to evaluate the impact of a disease or of treatment efficacy. Particularly in prosthodontics, several studies and systematic reviews have demonstrated that partial and conventional complete dentures significantly improved OHRQoL, especially concerning aesthetics and function. Qualities of life include the subjective sense of physical and/or mental well-being. In its broadest and most inclusive sense, it is sometimes referred to as “life satisfaction”.Bio-functionality tests are employed to investigate theprevalence of missing teeth and prosthodontic replacements in South Indian adult population using a hierarchical dental functional classification system. The paper aims to evaluate quality of life in patients with dental prosthesis done in south Indian population - Chennai, Tamilnadu: an epidemiological survey. The reasons for measuring HRQOL and functional status are that they provide a means of identifying and monitoring the impact of disease and interventions on the physical and mental health of elderly individuals as they themselves perceive this impact. Some of the causes of decreased HRQOL may be preventable and others are treatable with appropriate interventions. Short questionnaires that ask about these issues and are incorporated routinely into patient visits can provide information on HRQOL that alerts clinicians to changes that otherwise might go unrecognized. The number of “20 natural teeth” is the generally accepted WHO operative criterion for a functional natural dentition for adequate bio-functionality. In conclusion Quality of life is certainly disturbed in complete/partial edentulism. It includes in all aspect from psychological to functional.
Key Words: Edentulism, Chennai, OHRQoL, Prosthodontics
INTRODUCTION
Indian society is aging faster than most Western and Asian countries. People 60 years and older constitute 10 % of the Indian population, according to the 2017 India Ageing report. Maintaining good health and quality of life (QOL) is essential for the benefit of both individuals and society. Moreover, a growing number of elderly people are opting to spend the last years of their lives in long-term care facilities Grbich et al., 2005 and[1] Hirakawa et al., 2007.[2] Dental health care in long-term facilities, however, has repeatedly been documented as being inadequate Margaret et al., 2007 and[3] Ünlüer et al., 2007.[4] Studies have reported the effects of dental care on health status in the elderly. Yoneyama et al., 2002,[5] reported that improving dental health could lower the risk of respiratory infections, while Watando et al., 2004,[6] suggested that intensive oral care reduced the incidence of pneumonia by improving the cough reflex sensitivity in those who were physically disabled or suffering from mental deterioration. Yoshino et al., 2001,[7] showed an improvement in the QOL with intensive oral care among elderly nursing home patients with dysphagia due to cerebrovascular disease. Their finding suggested that oral care reduced the risk of pneumonia by improving the swallowing reflex, overall functional status, and quality of living. Eating begins from the anticipatory stage and proceeds through preparatory, lingual, pharyngeal, and esophageal stages Leopold and Kagel, 1983.[8] Maintaining or improving oral function with dental treatments also might improve QOL, but the effects of dental treatments on the QOL in the elderly have not been sufficiently examined. Impairment of oral health has a negative impact on the QOL of the elderly Mariño et al., 2008.[9] Some studies have found that their ability to function daily is an important determinant of the QOL of elderly home residents Tseng and Wang, 2001.[10] Therefore, we focused on this relationship and conducted a controlled study to determine whether dental treatments affect the QOL and in institutionalized elderly.
METHODOLOGY
Subjects and Study Design
This was a controlled study conducted at old age homes in Chennai, India, in 2018 for for 2 months. The study consisted of two phases: Subject screening and enrollment; outcome data were collected after the initial assessment. The subject screening was the selection of eligible subjects who met the criteria and those subjects who expressed willingness to participate were enrolled. Those who met the following two criteria were eligible for participation: Residence in the facility for at least 30 days and an age of 50 years or above. Written informed consent was obtained from all patients. The staff in the research administration office allocated the subjects into two groups in terms of their gender, age, and independence levels based on their financial/physical dependence.
Data Collection
In this study, QOL was assessed using the Kemper-Gascon Global Health and Well-being questionnaire personal well-being index (PWI). The PWI is a 9-item, 10-point scale that measures a patient’s ability to perform common daily tasks. It suggests that health-related QOL be defined as a person’s assessment of how the following affect his or her well-being. This includes functional factors, psychological factors, social factors, and the experience of pain/discomfort. When these considerations center on orofacial concerns, oral health-related QOL is assessed. The PWI contains nine questions. Each question has a score between 1 and 10, and the total score for the nine questions is the PWI score (maximum 90 and minimum 9). One of its strengths is its ability to reveal the psychosocial impact of oral health. The PWI data were collected at visit made to institutions information regarding daily life, such as diet and oral health behavior, spiritual well-being was provided by the residents. Oral health status in subjects at baseline was assessed.
Statistical Analysis
The differences in the demographic characteristics of the two groups at baseline were analyzed using the Chi-square – test for the association of edentulism. Two measurements in the edentulism and achieving in life scores were compared using Pearson’s correlation. All p-values were two-sided, and statistical significance was set at 0.05. All the analyses were performed using SPSS for Windows, version 14.0 (Statistical Product and Service Solutions, Chicago, IL, USA).
RESULTS
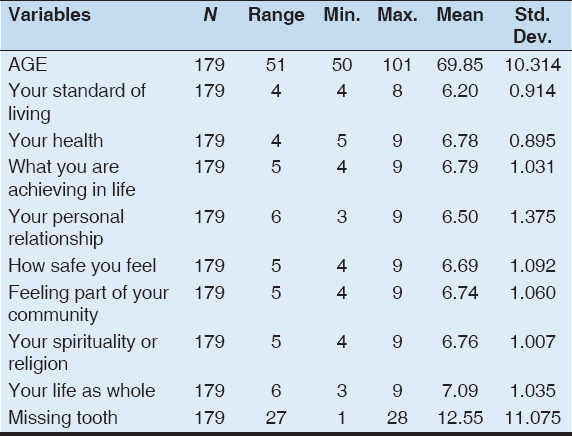
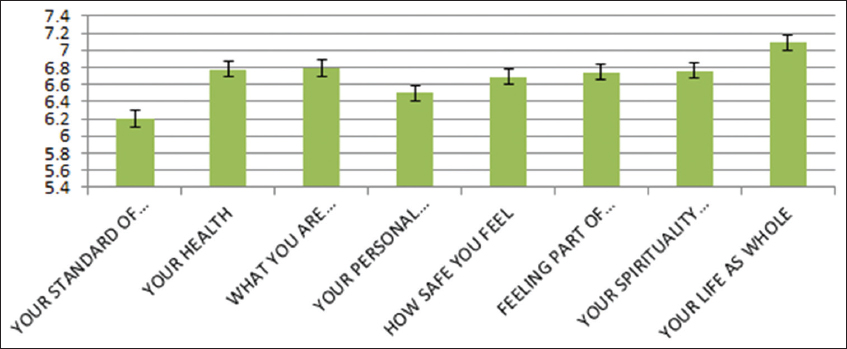
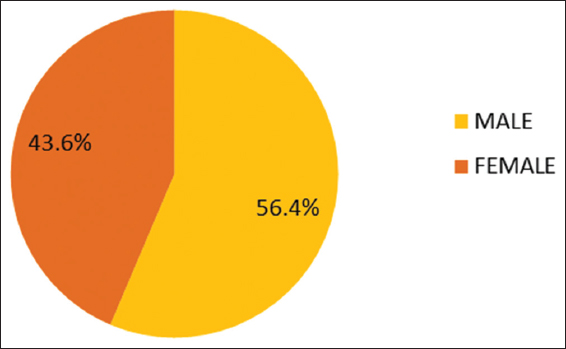
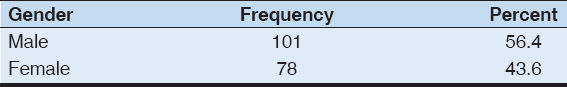
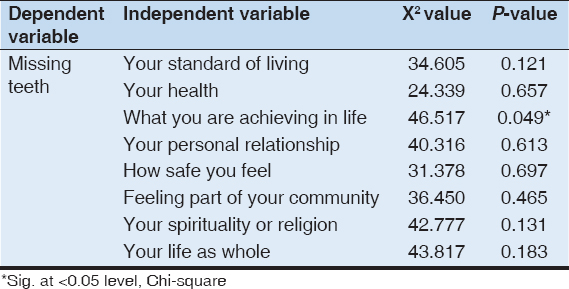
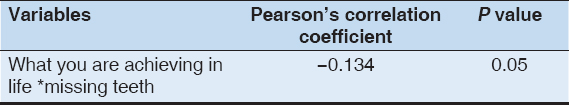
In this study, 179 subjects (101 men and 78 women) were examined for QOL. The results revealed that the average age was 51 with minimum age of 50 and maximum of 101. Their mean and standard deviation are shown in Table 1 and Figure 1. The gender distribution is show in Figure 2 and Table 2 the association of edentulism with various aspects of QOL, such as standard of living, health, achieving in life, personal relationship, feeling safe, feeling of belonging to a community, spirituality, and life as a whole. Table 3 shows the association of edentulism with questionnaire. Table 4 represents the correlation of achieving in life and edentulism. There was a significant association found between edentulism and achieving in life. Further, Pearson’s correlation revealed a weak negative correlation between the same.
Table 1: Mean and Standard deviation of questionnaire among the study population
Figure 1: Mean and standard deviation of questionnaire among the study population
Figure 2: Gender distribution among the study population
Table 2: Gender distribution among the study population
Table 3: Association of edentulism with questionnaire
Table 4: Correlation of achieving in life and edentulism
Inference: There is no significant association between all variables and missing teeth, except what you are achieving in life with P = 0.049.
Inference: There is a weak negative significant correlation between achieving in life and edentulism
DISCUSSION
In this controlled, 6-week study, we found that the dental treatments for institutionalized elderly increased the oral health-related QOL and the expression function in the ADL. No significant beneficial effects on feeding or transfer function were found, while dressing function tended to increase. To the best of our knowledge, this is the first controlled study involving nursing home residents to show that dental treatments influence the ADL and QOL. With old age, increased dependency affects the QOL negatively. Arslantas et al., 2009,[11] indicated that medico-social services for elderly people needed to be prioritized to improve the QOL and health training. For elderly residents of nursing homes, in addition to receiving good care and maintaining a strong physical condition and a healthy mental state, preserving QOL is important Poole and Kan, 2003.[12] Zanocchi et al., 2008,[13] reported that chronic pain in institutionalized elderly was common and worsened their QOL. In our study, as the importance of assessing and managing pain was emphasized, reducing chronic pain by dental treatments could help to improve the QOL in some cases.
The increase of expression scores in the intervention group was significantly higher than those in the control group, while these scores in both groups improved. The expression can be a sensitive marker of events in everyday life. The dental treatment likely restored the subject’s oral function and led to improved expression. Furthermore, conducting the intervention might have stimulated the subjects in their daily life. The difference between groups might have arisen from the ADL status just before the intervention. The expression was lower than other items in the intervention group at baseline. Other scores, including feeding, did not improve significantly. These results suggest the difficulty in detecting small changes in the ADL with intervention in elderly people who have maintained a certain level of independence. The QOL increased significantly with the intervention. Dental treatments, such as making dentures, often need time to alter the patients’ symptoms and allow them to recover from oral dysfunction. Therefore, studies using subjective indicators must follow to evaluate the effects of dental treatments. Feeding was not directly linked to the improvement in the QOL. Most of the dental treatments in this study could not be interventions that changed the subjects’ eating function dramatically. In addition, all subjects had maintained the pre-intervention level of oral intake, which might have contributed to the lack of a statistically significant change in the feeding scores. The dental staffs can contribute to and facilitate improvement in nursing home residents’ QOL by helping them maintain or regain optimum oral health and function, which contributes to their well-being and general health by furthering nutrition, alleviating pain and discomfort, and increasing personal esteem and social acceptability Schembri and Fiske, 2005.[14] Meanwhile, Pyle, 2005,[15] indicated that oral health continued to have a low priority in nursing facilities. They also suggested that continuing efforts to improve oral health and educate long-term care professionals about the influence of oral health on general health were critical for managing the oral health of future generations of aging adults. Our findings provided further evidence that dental professionals need to recognize the importance of residential home care.
We targeted nursing home residents in this study. A previous study also revealed the impairment of oral health and oral health care needs for community-dwelling elderly people with disabilities Saunders and Friedman, 2007.[16] Further studies investigating the effects of dental treatments on ADL and QOL in various settings are needed. They will provide useful clues for future health care policy.
A few limitations to this study warrant consideration. First, the subjects were not allocated randomly into the two groups.
However, the basic characteristics of the groups were similar and the analysis made statistical adjustments if necessary. Second, the dropout rate in this study was 17% (five subjects), although it did not differ significantly between the two groups. The reason for the withdrawal of three of the five was worsening health, which could not be prevented. While one subject in the intervention group was analyzed in the control group, the intention-to-treat analysis showed that the results were the same as those for each protocol.
In addition, the sample size was small, and we could not conduct a stratified analysis of gender or other factors. Continuous efforts for further research are warranted to confirm these findings.
In conclusion, our findings indicated that dental treatments for the institutionalized Japanese elderly improved the oral health-related QOL and the expression function in the ADL. Promoting dental care service at nursing facilities may be beneficial for maintaining residents’ QOL.
CONCLUSION
QOL is certainly disturbed in complete/partial edentulism. It includes all aspect from psychological to functional. This study was conducted at old age homes in Chennai, India, in 2018 for for 2 months to find the QOL in patients with dental prosthesis using a questionnaire. There was a significant association found between edentulism and achieving in life. Further, Pearson’s correlation revealed a weak negative correlation between the same.
DECLARATION
Ethics approval and consent to participate were procured before the study from the Institutional Ethical Committee, consent for publication was also procured. Further, there are no competing interests. No funding was provided by any agency. The author (Dr. Gayathri) carried out the research and guided by Dr. Sharmila. Finally, the authors also acknowledge the institute for providing all support and encouragement to carry out the study.
REFERENCES
1. Grbich C, Maddocks I, Parker D, Brown M, Willis E, Piller N,
2. Hirakawa Y, Kuzuya M, Uemura K. Opinion survey of nursing or caring staff at long-term care facilities about end-of-life care provision and staff education. Arch Gerontol Geriatr 2009;49:43-8.
3. Margaret S, Williams C, Kennedy C, Louise M, Stephen T, Jeremy B. Oral health care and status of elderly care home residents in Glasgow. Community Dent Health 2007;24:37-42.
4. Ünlüer S, Gökalp S, Doğan BG. Oral Health Status of the Elderly in a Residential Home in Turkey. Gerodontology 2007;24:22-9.
5. Yoneyama T, Yoshida M, Ohrui T, Mukaiyama H, Okamoto H, Hoshiba K,
6. Watando A, Ebihara S, Ebihara T, Okazaki T, Takahashi H, Asada M,
7. Yoshino A, Ebihara T, Ebihara S, Fuji H, Sasaki H. Daily oral care and risk factors for pneumonia among elderly nursing home patients. JAMA 2001;286:2235-6.
8. Leopold NA, Kagel MC. Swallowing, ingestion and dysphagia:A reappraisal. Arch Phys Med Rehabil 1983;64:371-3.
9. Mariño R, Schofield M, Wright C, Calache H, Minichiello V. Self-reported and clinically determined oral health status predictors for quality of life in dentate older migrant adults. 2008;36:85-94.
10. Tseng ZS, Wang RH. Quality of life and related factors among elderly nursing home residents in Southern Taiwan. Public Health Nurs 2001;18:304-11.
11. Arslantas D, Unsal A, Metintas S, Koc F, Arslantas A. Life quality and daily life activities of elderly people in rural areas, Eskişehir (Turkey). Arch Gerontol Geriatr 2009;48:127-31.
12. Poole BJ, Kan MJ. Working-memory capacity predicts the executive control of visual search among distractors:The influences of sustained and selective attention. Q J Exp Psychol 2009;62:1430-54.
13. Zanocchi M, Maero B, Nicola E, Martinelli E, Luppino A, Gonella M,
14. Schembri A, Fiske J. Oral health and dental care facilities in Maltese residential homes. Gerodontology 2005;22:143-50.
15. Pyle MA. Nursing home executive directors'perception of oral care in long-term care facilities. Spec Care Dentist 2005;25:111-7.
16. Saunders R, Friedman B. Oral health conditions of community-dwelling cognitively intact elderly persons with disabilities. Gerodontology 2007;24:67-76.